Author: Dr. Farhat Naz
Wilson’s Disease, Case History, introduction, genetics, Clinical features, workup, management, prognosis.
Case Scenario:
Fatima, a 27-year-old female, presented in emergency with a three-day history of fever. She had jerky movements of the body. She also experienced an inability to walk, eat, and sit.
The patient developed high grade intermittent fever three days ago, according to mother. After that, she got intense tremors of the body. She developed inability to speak, move and eat. The fits were not linked to frothing, tongue bite or incontinence of urine.
Her past history is significant for a psychiatric illness starting 3 years ago. She then developed tremors of the hands. The doctor prescribed medications for this, but she experienced little relief in her symptoms. She was unable to walk and eat without support for the last one year. Her latest deterioration started after her recent episode of fever. Jerking of the body worsened until it went out of control. She needed hospitalization.
Apart from her fever and tremors, she had no other neurological symptoms like headache and altered consciousness. However, she is also a victim of psychiatric illness that started 3 years ago.
Her family history is significant for liver disease and movement disorder. Her elder brother died of liver disease and the other one died of disability and tremor. Her paternal cousins have similar type of disease. Her brother and cousins got their assessment done from Jinnah Hospital Karachi. Their record showed end stage liver disease and low ceruloplasmin levels. They also had high 24 hours urine excretion of copper suggesting the diagnosis of Wilson’s Disease. Her brother is on chelation therapy with D- penicillamine and Zinc acetate supplements. She did not undergo any workup for Wilson’s disease herself. However, due to a strong family history of the disease, she was started on chelation therapy with D- penicillamine. She showed significant improvement within days.
Among her alive siblings, one brother and one sister are suffering from liver disease, two of siblings are normal. Parents had cousin marriage and they are normal.
She visited doctors for her disease and they prescribed her antidepressants, procyclidine and levodopa +carbidopa for temors. She was not previously hospitalized.
She could not go to school for formal education but studied at home. She got married to her paternal cousin 10 years ago. She remained issueless in her 7 years of marriage. She was divorced 3 years ago. Her mental illness started then and her behaviour change led to her divorce.
She is staying with her parents and father is the only earner of family. She is dependent on her mother for eating, moving and cannot take care of herself.
Her economic condition is average. She lives with parents who have their own house and land, which is quite enough for their living. However, her illness and her siblings’ illness have posed an economic burden to the family.
On Examination:
She is a young conscious lady with rigorous tremors involving head (titubation) and the whole body. Upon neurological examination, her muscle tone is increased and having cog wheel type of rigidity. Hand tremors get worse on intention. Typical wing-beating tremors appear while attempting to hold the arms in an outstretched or bent position. Overall she had the following neurological problems:
Tremors
Difficulty with coordination and
balance
Slurred speech
Muscle stiffness and weakness
Cognitive impairment Behavioral changes
social and emotional impact:
Fatima’s illness has taken a toll on her personal life, leading to the dissolution of her marriage.
She faces the added emotional burden of infertility, which can be attributed to her illness.
The strong family history of the disease and its impact on her relatives have likely caused significant emotional distress.
Workup:
1. Serum ceruloplasmin level:
8 vmg/dL (normal range: 20-35 mg/dL)
2. 24-hour urinary copper excretion:
200 µg/24h (normal range: <40 µg/24h)
3. Liver function tests:
Serum ALT (alanine aminotransferase): 45 U/L (normal range: 7-56 U/L)
Serum AST (aspartate aminotransferase): 38 U/L (normal range: 10-40 U/L)
Serum alkaline phosphatase: 120 U/L (normal range: 30-120 U/L)
Serum total bilirubin: 0.8 mg/dL (normal range: 0.2-1.2 mg/dL)
4. Complete blood count:
Hemoglobin: 12 g/dL (normal range: 12-16 g/dL)
White blood cell count: 6,500/μL (normal range: 4,500-11,000/μL)
Platelet count: 250,000/μL (normal range: 150,000-400,000/μL
5. Electrolytes:
Serum sodium: 140 mEq/L (normal range: 135-145 mEq/L)
Serum potassium: 4.2 mEq/L (normal range: 3.5-5.0 mEq/L)
Serum calcium: 9.0 mg/dL (normal range: 8.5-10.5 mg/dL)
6. Renal function tests:
Serum creatinine: 0.8 mg/dL (normal range: 0.6-1.1 mg/dL)
Blood urea nitrogen (BUN): 15 mg/dL (normal range: 7-20 mg/dL)
7.Coagulation profile:
Prothrombin time (PT): 12 seconds (normal range: 11-13 seconds)
International normalized ratio (INR): 1.1 (normal range: 0.8-1.2)
8. Genetic testing:
Not performed, the patient was diagnosed on the basis of strong family history, lab tests and imaging.
9. Imaging: MRI of the brain:
T2-weighted and FLAIR sequences reveal hyperintense signals in the basal ganglia, predominantly involving the putamen bilaterally.
10. Slit-Lamp Examination:
Evaluation of the anterior segment reveals a characteristic copper-colored ring encircling the iris (KF Ring), more pronounced in the superior and inferior quadrants.
11. Liver Biopsy:
Not done and the diagnosis was established on lab tests and imaging.
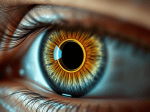
keyser Fleisher Ring in Wilson’s Disease
What is Wilson’s Disease, and how is it inherited?
Wilson’s disease is a rare genetic disorder. It causes the accumulation of copper in various organs of the body. This mainly affects the liver and brain. It is inherited in an autosomal recessive manner. A person needs to inherit two mutated copies of the ATP7B gene. They receive one copy from each parent to develop the disease.
What are the common symptoms and signs of Wilson’s Disease?
Common symptoms and signs include:
- Fatigue
- Jaundice (yellowing of the skin and eyes)
- Swelling in the abdomen (ascites)
- Swelling in the legs (edema)
- Easy bruising
- Neurological symptoms such as tremors, difficulty walking or speaking, and involuntary movements
- Behavioral changes, such as mood swings, depression, or psychosis
- Kayser-Fleischer rings (copper deposits in the eyes, visible as a golden-brown ring around the cornea)
Early detection and treatment are crucial in managing Wilson’s Disease effectively.
At what age Wilson’s Disease is manifested?
Wilson’s disease can manifest at any age. It most commonly becomes apparent during adolescence or early adulthood. The typical age range is between 10 and 30. However, it can also present later in life, including in middle-aged and older adults. The age of onset can vary widely among individuals, and the symptoms and severity of the disease can also vary. In some cases, Wilson’s disease may be diagnosed in childhood. Diagnosis is more likely if there is a family history of the condition. It is also likely if symptoms such as liver dysfunction or neurological problems appear early.
How Wilson’s disease is diagnosed?
Wilson’s Disease can be diagnosed through a combination of medical history, physical examination, and various tests. Here are some common diagnostic methods:
- Blood tests: Blood tests can measure levels of ceruloplasmin (a protein that carries copper in the blood) and copper. In Wilson’s Disease, ceruloplasmin levels are often low, and copper levels are usually elevated.
- Urine tests: A 24-hour urine collection can measure the amount of copper excreted. In Wilson’s Disease, urinary copper levels are typically elevated.
- Liver function tests: These tests can reveal abnormalities in liver enzymes, indicating liver damage or dysfunction.
- Genetic testing: Genetic testing can identify mutations in the ATP7B gene, which is responsible for regulating copper metabolism. However, not all individuals with Wilson’s Disease have identifiable mutations in this gene.
- Liver biopsy: A small sample of liver tissue is taken. It is then examined under a microscope to assess the amount of copper present.
- Liver biopsy may also reveal signs of liver damage or cirrhosis.
- Eye examination: A slit-lamp examination can detect Kayser-Fleischer rings. These rings indicate copper deposition in the eyes. This is a hallmark of Wilson’s Disease.
What are the psychiatric symptoms of Wilson’s disease?
Psychiatric symptoms can include mood swings, depression, anxiety, personality changes, psychosis, and cognitive impairment. These symptoms can vary widely among individuals. They may occur alongside physical manifestations such as liver disease. Neurological symptoms can include tremors and difficulty with movement. Early detection and treatment are crucial in managing the condition and preventing irreversible damage.
What are neurological manifestations of Wilson’s disease?
- Tremors and Movement Disorders:
Action Tremors: Wilson’s Disease often presents with action tremors. These are tremors that occur during voluntary movements. Examples include reaching for an object or holding a utensil.
Dystonia: This neurological disorder results in sustained muscle contractions, leading to abnormal postures and repetitive, twisting movements. Dystonia can affect various body parts, including the hands and face.
- Dysarthria and Dysphagia:
Dysarthria: Wilson’s Disease can cause dysarthria, a speech disorder characterized by slurred or difficult- to-understand speech. This condition can make communication challenging.
Dysphagia: Difficulty in swallowing, known as dysphagia, can also occur in Wilson’s Disease, leading to problems with eating and drinking.
- Rigidity and Bradykinesia:
Patients may experience muscle rigidity and bradykinesia, which are characteristic features of Parkinsonism. These symptoms can significantly affect mobility and daily activities.
- Personality and Behavioral Changes:
Wilson’s Disease can lead to personality changes, mood disturbances, and behavioral abnormalities. Patients may exhibit depression, anxiety, irritability, or even psychosis.
- Cognitive Impairment:
- Cognitive deficits can range from subtle difficulties with attention and memory to more severe impairments in executive functioning and reasoning.
In advanced cases, cognitive decline may resemble dementia.
- Kayser-Fleischer Rings:
These are characteristic copper deposits in the cornea of the eye,
visible during an eye examination.
They are a diagnostic hallmark of Wilson’s Disease and result from copper build-up in the eye.
- Seizures:
:Although less common, seizures can occur in Wilson’s Disease patients, particularly when copper levels are elevated.
- Pseudobulbar Symptoms:
Pseudobulbar symptoms, such as emotional lability (inappropriate laughing or crying), can also manifest due to the involvement of certain brain regions.
- Gait Disturbances:
Problems with coordination and balance can lead to gait disturbances, making walking difficult and increasing the risk of falls.
Diagnosing neurological manifestations of Wilson’s Disease often involves different methods. These include a clinical evaluation. Imaging studies, such as brain MRI, are also used. Copper-related blood tests are another important component. Genetic testing is essential to confirm the presence of ATP7B gene mutation.
How Wilson’s disease affects the liver?
Hepatic manifestations are often the initial and most prominent features of this condition. In the liver, copper buildup can cause inflammation. It can damage liver cells and ultimately lead to conditions like hepatitis, cirrhosis, or liver failure.
How Wilson’s disease is treated?
here’s a comprehensive treatment outline for Wilson’s disease:
1. Copper Chelation Therapy:
Initial treatment involves medications to remove excess copper from the body.
Common medications include D- penicillamine, trientine, or zinc acetate.
These medications bind to copper, allowing it to be excreted in urine or stool.
2. Zinc Supplementation:
- Zinc blocks copper absorption in the intestines.
- It is often used as maintenance therapy to prevent copper reaccumulation.
- Zinc supplements are typically taken orally.
3. Dietary Restrictions:
- Patients are advised to avoid foods high in copper, such as shellfish, nuts, chocolate, and mushrooms.
- Drinking water from copper pipes should also be avoided.
4. Regular Monitoring:
- Patients require regular monitoring of copper levels in the blood and urine to assess treatment effectiveness.
- Liver function tests and neurological evaluations also performed.
5. Liver Transplant:
- In severe cases of liver failure or when medical therapy fails, liver transplantation is necessary.
- This involves replacing the diseased liver with a healthy donor liver.
6. Psychological Support:
- Living with a chronic condition like Wilson’s disease can be challenging. Psychological support may help patients and their families. Counseling may also be beneficial.
- Support groups can also provide valuable emotional support and practical advice.
7. Genetic Counseling:
- Wilson’s disease is a genetic disorder. Genetic counseling may be offered to individuals and families. This helps them understand the inheritance pattern. It also allows discussion about risks and options for family planning.
8. Regular Follow-up:
- Long-term management of Wilson’s disease requires regular follow-up appointments with healthcare providers. These appointments check treatment effectiveness. They also manage any complications and adjust therapy as needed.
What is the role of liver transplant in Wilson’s disease?
Liver transplant is crucial in managing Wilson’s disease. It is particularly important in cases of severe liver failure. Additionally, it is needed when medical therapy fails to control symptoms effectively. Here are the indications and prognosis for liver transplant in Wilson’s disease:
Indications for Liver Transplant:
- End-Stage Liver Disease: When Wilson’s disease progresses to end-stage liver disease, it is characterized by severe liver damage or cirrhosis. A liver transplant may be necessary to prevent liver failure and associated complications.
- Failure of Medical Therapy: In some cases, medical therapy with copper chelators may not adequately control copper levels. Zinc supplementation might also fail to halt disease progression. Liver transplant becomes a viable option when medical therapy fails.
- Neurological Complications: Although less common, neurological complications of Wilson’s disease may occur. These include severe movement disorders or cognitive impairment. A liver transplant may be warranted if they are refractory to medical management.
Prognosis:
- Improved Survival: Liver transplant can significantly improve survival and quality of life for patients with Wilson’s disease. This is especially true for those with advanced liver disease. It also benefits patients with complications that do not respond to medical therapy.
- Resolution of Symptoms: Liver transplant typically resolves liver-related symptoms. These include jaundice, ascites, and hepatic encephalopathy. This procedure allows patients to regain normal liver function.
- Long-Term Management: After liver transplant, patients require lifelong immunosuppressive medications to prevent rejection of the transplanted liver. The prognosis is generally favorable for patients with Wilson’s disease who undergo a liver transplant. This is due to proper management and adherence to medical treatment.
- Potential Complications: Like any major surgery, liver transplant carries risks of complications. These include infection, rejection, and adverse effects of immunosuppressive medications. However, with advancements in surgical techniques and post-transplant care, the risk of complications has decreased over time.
Liver transplant is a life-saving intervention for patients with Wilson’s disease. It is crucial for those who have advanced liver disease or fail to respond to medical therapy. It offers the potential for improved survival, resolution of symptoms, and better quality of life.
How the treatment response in monitored in Wilson’s Disease?
Treatment response in Wilson’s disease is monitored through a combination of clinical, biochemical, and imaging assessments. Biochemical markers are commonly used to evaluate treatment efficacy. These include serum ceruloplasmin levels, urinary copper excretion, and liver function tests. Decreased serum ceruloplasmin levels and reduced urinary copper excretion indicate inadequate treatment response. Normalization of these parameters suggests successful treatment. Liver function tests include serum transaminases and bilirubin levels. These tests are monitored to assess hepatic function. They help to assess the progression of liver damage.
Imaging studies such as liver ultrasound, MRI, or CT scans may be used to evaluate the extent of liver damage. These scans also check for hepatic nodules or cirrhosis. Additionally, brain imaging studies such as MRI detect copper accumulation in the basal ganglia. This is characteristic of neurological involvement in Wilson’s disease.
Regular clinical assessments are essential to monitor symptoms such as fatigue, jaundice, neurological manifestations, and psychiatric symptoms. Objective scoring systems are helpful. One example is the Unified Wilson’s Disease Rating Scale (UWDRS). They can assist in measuring the severity of the disease. Another important tool is the Global Assessment Scale for Wilson’s Disease (GAS-WD). They can track changes in symptoms over time.
What is prognosis of Wilson’s disease?
With early diagnosis and appropriate treatment, the prognosis for Wilson’s Disease is generally good. Lifelong management is often required, but individuals can lead normal lives. Untreated, the disease can be fatal due to liver failure or neurological complications.
What are the diagnostic and prognostic scores used in Wilson’s Disease?
Two important scores used in Wilson’s Disease are:
- Diagnostic Score:
- The Leipzig Score:
- The Leipzig score is a tool used in the diagnosis of Wilson’s disease, a genetic disorder affecting copper metabolism. It helps clinicians assess the likelihood of Wilson’s disease based on clinical features, laboratory findings, and genetic testing results. The score ranges from 0 to 13, with higher scores indicating a greater probability of Wilson’s disease. It considers factors such as age and ceruloplasmin levels. It also includes urinary copper excretion, the presence of Kayser-Fleischer rings (a characteristic eye finding), and genetic testing results. A higher Leipzig score suggests a higher probability of Wilson’s disease, prompting further evaluation and potentially confirming the diagnosis.
- Prognostic Score:
- The Model for End-Stage Liver Disease (MELD) score:
- The Model for End-Stage Liver Disease (MELD) score is a numerical scale. It assesses the severity of liver disease. It also predicts the short-term mortality risk for patients with liver dysfunction. It is primarily used to prioritize patients for liver transplantation. The MELD score uses three laboratory values. These are serum bilirubin, serum creatinine, and international normalized ratio (INR) for prothrombin time. The formula for calculating the MELD score is:
- MELD Score = 3.78 × In(Serum Bilirubin [mg/dL]) + 11.2 × In(INR) + 9.57 × In(Serum Creatinine [mg/dL]) + 6.43
- The score ranges from 6 to 40. Higher scores indicate more severe liver dysfunction. They also show a higher risk of mortality. Patients with higher MELD scores are prioritized for liver transplantation. They have a greater risk of dying without a transplant.
- The MELD score has become the standard tool for organ allocation in many countries. It can objectively assess disease severity. It also predicts short-term mortality in patients with liver disease.
What disciplines are involved in management of Wilson’s Disease?
The management of Wilson’s Disease typically involves a multidisciplinary approach. Here are the disciplines commonly involved:
- Gastroenterology/Hepatology: Specialists in these fields are crucial. They assist in diagnosing and managing the liver manifestations of Wilson’s Disease, such as hepatomegaly, jaundice, and liver dysfunction.
- Neurology: Neurologists play a significant role in assessing neurological symptoms associated with Wilson’s Disease. They treat movement disorders, tremors, dystonia, dysarthria, and cognitive impairment.
- Genetics: Genetic counselors can provide information about Wilson’s Disease. They offer support regarding its inheritance pattern. Counselors can also discuss genetic testing and the implications for family members.
- Psychiatry/Psychology: Mental health professionals provide help with psychiatric symptoms often seen in Wilson’s Disease. These symptoms include depression, anxiety, and behavioral changes.
- Radiology: Radiologists interpret imaging studies such as MRI and CT scans. They assess for structural brain abnormalities. They also evaluate disease progression.
- Endocrinology: Consult endocrinologists for the management of endocrine disorders linked to Wilson’s Disease. These may include thyroid function abnormalities.
- Nutrition/Dietetics: Dietitians can provide dietary recommendations. They can advise on copper intake restriction. They may also suggest supplementation with zinc, which helps prevent copper absorption in the intestines.
- Occupational Therapy/Physical Therapy: These disciplines help patients manage physical disabilities, improve motor function, and maintain independence in daily activities.
- Speech Therapy: Speech therapists assist in managing speech and swallowing difficulties. These issues can occur due to neurological involvement in Wilson’s Disease.
- Social Work: Social workers provide support and resources. They assist with navigating healthcare systems and financial concerns. They also help with psychosocial challenges associated with chronic illness. Collaboration among these various disciplines ensures comprehensive care for individuals with Wilson’s Disease, addressing both hepatic and neurological manifestations.

