Scleroderma Case history, introduction, types, aetiology, investigations,management, prognosis.
By: Dr. Farhat Naz
Co author: Dr. Elaf Aslam

Case Study:
30 years old female known case of Scleroderma since last 9 years presented in emergency with the complaints of chest pain, shortness of breath, dry cough and low grade fever for one week. The shortness of breath occured mostly on exertion but it has worsened now for last one wèek.
She had past histoy of dysphagia to solids for last 1 year with resulting decreased oral intake.
Her problem started 9 years ago when she started having whitish discoloration and pain of fingers, the skin of the fingers progressively became tightened and few of her fingers developed black discoloration followed by auto amputation of digits.
She also has history of stiffness of joints. She consulted doctor for her initial problems where the diagnosis of scleroderma was made.
She used moisturizing creams for her dry and tight skin and used ibuprofen and Methotrexate for pain and stiffness.
On Examination:
Vital Signs: BP: 85/60mmHg, Pulse was 105/min, SPO2: 85% and was afebrile.
~On General look:
Patient was oriented and alert having special facial appearance with tight shiny skin and loss of forehead wrinkles. She had fish like mouth, beaked nose and pigmentation on face. She had telangieactasia on face (right cheek).

She had calcinosis on interphalangeal joints, hard skin, sclerodactyly and peripheral digital gangrene with auto amputation of fingertips.

Examination of feet also revealed auto amputation of digits, but no active gangrene.

~SYSTEMIC EXAMINATION:
Chest: decreased air entry in lower zones bilaterally, fine crepitations in both upper and middle lung zone.
CVS: Tachycardia with S3 gallop, raised JVP, mild peripheral odema.
CNS: GCS 15/15, no motor or sensory deficit.
Abdomen: Mild epigastric tenderness.
Investigations:
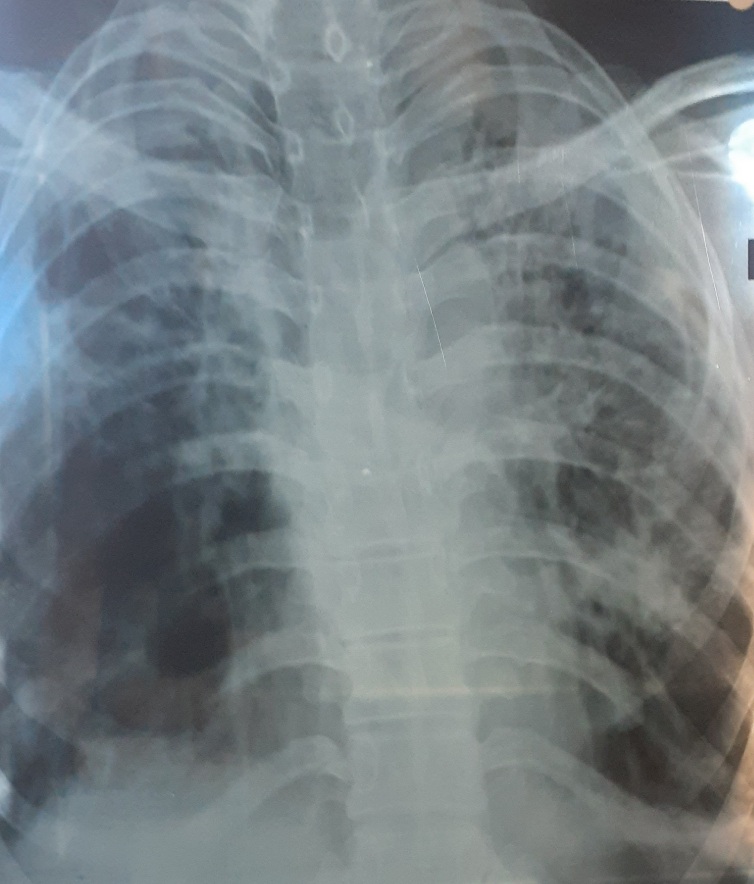
~Chest Xray: revealed fibrotic changes in both lung field, more marked in left lung.
~Echocardiography showed mild Tricuspid regurgitation and Right ventricular overload and increased right ventricular systolic pressure (RVS P)suggesting mild Pulmonary Hypertension with ejection fraction of 58%.
~USG of Abdomen/pelvis showed mild left pleural effusion and bilaterally increased renal echogenicity.
~Labs revealed;
ESR ~ 70 mm/Ist hour, Complete blood count, renal and liver functions were normal.
Patient was treated for pulmonary hypertension and right heart failure.
What treatment can be offered to prevent further lung fibrosis and deterioration?
In this article, we will discuss scleroderma under following headings;
What is scleroderma?
Who develops scleroderma?
What is pathophysiology of Scleroderma?
What are the types of scleroderma?
What are clinical features of scleroderma?
What is Morphoea?
What is CREST syndrome?
What is Diffuse Cutaneous Scleroderma?
What investigations are performed in scleroderma?
What is the role of imaging in scleroderma?
What is management of scleroderma?
What are the advanced complications of scleroderma?
Lung involvement in scleroderma
kidney involvement in scleroderma
Dysphagia in scleroderma
What is life expectancy in Scleroderma?
What is scleroderma?
Sclerderma is a disease of autoimmune aetiology characterized by tightness and scarring of skin, blood vessels and internal organs due to widespread proliferation of fibrous tissue, leading to specific manifestations of the disease.
Who develops scleroderma?
Anyone can develop scleroderma, but is mostly affects females 30-50 years of age. African American develop the disease earlier with more extensive systemic involvement.
What is pathogenesis of Scleroderma?
As the scleroderma is an auto immune disease, the normal immune mechasinsm of the body is altered leading to abnormal interaction between endothelial cells, fibroblasts, B and T lymphocytes.
Three basic mechanism in development of scleroderma include
- Vascular dysfunction
- Immune alteration
- Fibroblast activation
The exact trigger of the disease is unknown but the interaction of genetic and environmrntal factors play a role. The endothelial cells of blood vessels are damaged leading to release of endothelin 1, Endothelin 1 is a potent vasoconstrictor and activator of fibroblasts and myoblasts, causing the manifestations of the disease.
What are the types of scleroderma?
There are two major types of scleroderma:
- 1. Localized Scleroderma: which is localized to skin and subcutaneous tissue. It may take the form of thickened patches called Morphoea or develop in Linear form down the arms, legs or face (mostly affecting chidren).
- 2. Systemic scleroderma: also known as systemic sclerosis. This type involves skin and internal organs both. This form is further divided into Limited Cutaneous and diffuse forms with involvement of internal organs like heart, kidney and digestive system.
- 3. Sine scleroderma:This is third rare type of scleroderma, which only involves the internal organs but sparing the skin.
What are clinical features of scleroderma?
Scleroderma is a chronic autoimmune disease that affects the skin and connective tissues. The clinical features of scleroderma vary depending on the type and severity of the disease, but may include:
- Skin thickening: The skin may become thick and tight, with a leathery appearance, most commonly affecting the fingers, hands, face, and legs.
- Raynaud’s phenomenon: Raynaud’s phenomenon is a condition characterized by painful, white or blue fingers or toes in response to cold or stress.
- Joint pain and stiffness: Joint pain and stiffness may occur, especially in the fingers and hands.
- Muscle disease: Muscle disease in Scleroderma can be inflammatory or non inflammatory, it causes muscle pain and weakness.
- Fatigue: Fatigue is a common symptom of scleroderma, which can be severe and impact daily activities.
- Anemia: Anemia is common symptom in scleroderma and is a mojor contributing factor in causing fatigue.
- Dysphagia/GIT: Difficulty in swallowing, also known as dysphagia, may occur as a result of esophageal involvement in scleroderma. Any part of GIT can be involved in scleroderma, leading to reflux, malabsorption, weight loss and bleeding from stomach due to a condition called Gastric Antral Vascular Ectesia (GAVE), having the appearance of ‘Watermelon stomach’ on endoscopy.
- Calcinosis: Calcinosis is the accumulation of calcium deposits in the skin or other tissues, which can cause pain and skin ulceration.
- Telangiectasia: Telangiectasia is the development of small blood vessels on the skin, which can become visible as red or blue lines.
- Lung involvement: Lung involvement, including interstitial lung disease and pulmonary arterial hypertension, is a serious complication of scleroderma and can lead to respiratory failure.
- Kidney involvement: Kidney involvement, including scleroderma renal crisis, is a serious complication of scleroderma and can lead to end- stage renal disease.
The clinical features of scleroderma can vary greatly between individuals and can change over time. It is important for individuals with scleroderma to be evaluated and treated by a specialist to ensure an accurate diagnosis and appropriate management.
What is Morphoea?
Morphoea is characterized by localized patches of hard shiny skin which sometimes involve underlying tendons and bones.
It is classified as localized form of scleroderma without organ involvement.
Treatment is with Corticosteroids, Methotrexate and ultravoilet UV phototherapy.

What is CREST syndrome?
It is characterized by the presence of the following symptoms:
Calcinosis: (formation of calcium deposits in the skin),
Raynaud’s phenomenon: (spasm of blood vessels in the fingers and toes)
Esophageal dysmotility: (difficulty swallowing)
Sclerodactyly: (thickening and tightening of the skin on the fingers and toes), and
Telangiectasia: (widening of small blood vessels near the surface of the skin).
All features of CREST syndrome are manifestations of limited cutaneous scleroderma, without systemic involvement.
What is Diffuse Cutaneous Scleroderma?
Diffuse cutaneous scleroderma is most extensive form of systemic sclerosis with more extensive skin involvement alongwith involvement of lungs, heart and kidneys, leading to life threatening complications of the disease.
What investigations are performed in scleroderma?
Diagnosing scleroderma typically involves a combination of medical history, physical examination, and various diagnostic tests. Some common investigations for scleroderma include:
- Blood tests: Blood tests can help evaluate for markers of inflammation, autoimmune activity, and organ involvement.
- Skin biopsy: A skin biopsy can help confirm the diagnosis of scleroderma and determine the type and severity of the disease.
- Imaging studies: Imaging studies, such as X-rays, MRI, and CT scans, can help evaluate for skin thickening, joint involvement, and organ involvement.
- Pulmonary function tests: Pulmonary function tests can help evaluate for lung involvement in individuals with scleroderma.
- Gastrointestinal tests: Gastrointestinal tests, such as esophageal manometry, can help evaluate for dysphagia and esophageal dysmotility in individuals with scleroderma.
- Kidney function tests: Kidney function tests, such as creatinine levels, can help evaluate for kidney involvement in individuals with scleroderma.
What is the role of Auto Immune profile in Scleroderma?
Autoimmune profile is a test that measures levels of antibodies in the blood to help diagnose autoimmune disorders such as scleroderma.
However, as with all tests, the results should be interpreted in conjunction with clinical symptoms and other diagnostic tests.
Antinuclear antibodies (ANA):
Antinuclear antibodies (ANA) are proteins that are produced by the immune system and attack the body’s own cells and tissues. ANA testing is a common blood test used to diagnose autoimmune diseases, including scleroderma.
In scleroderma, ANA are often present in high levels and can help diagnose the condition. ANA testing is not specific to scleroderma and can be positive in other autoimmune diseases as well, so further tests and clinical evaluation are usually necessary to confirm the diagnosis of scleroderma.
ANA testing is performed by taking a sample of blood and examining it under a microscope to detect the presence of ANA. A positive ANA test result indicates that the patient has an autoimmune disease, but it does not provide information about the type or severity of the disease.
There are number of antibodies associated with scleroderma and mostly a specific antibody is related to type a specific of Scleroderma.
Scleroderma antibodies are classified based on their sensitivity and specificity in the diagnosis of scleroderma:
Anticentromere antibodies (ACA) are considered to be highly specific for limited cutaneous scleroderma, but they have low sensitivity, meaning not all patients with limited cutaneous scleroderma will test positive for ACA.
Anti-Scl-70 (topoisomerase I) antibodies: are considered to be highly specific for diffuse cutaneous scleroderma, but they have moderate sensitivity, meaning not all patients with diffuse cutaneous scleroderma will test positive for Anti-Scl-70.
Anti-RNA polymerase III antibodies: are considered to be highly specific for systemic sclerosis (a type of scleroderma), but they have moderate sensitivity, meaning not all patients with systemic sclerosis will test positive for Anti-RNA polymerase
Anti-U3 RNP (also known as fibrillarin) antibodies: are considered to be highly specific for limited cutaneous scleroderma, but having low sensitivity, meaning not all patients with limited cutaneous scleroderma will test positive for Anti-U3 RNP.
It is important to note that the sensitivity and specificity of scleroderma antibodies can vary depending on the population studied and the laboratory methods used.
What is the role of imaging in scleroderma?
Imaging studies play a key role in the evaluation and management of scleroderma. The following are some of the imaging tests that may be used in scleroderma patients:
- Skin ultrasound: This test uses high-frequency sound waves to produce images of the skin, allowing for assessment of skin thickness and calcinosis.
- Chest X-ray: Chest X-rays can be used to evaluate for lung involvement, including interstitial lung disease, which can appear as hazy shadows on the X-ray.
- CT Chest: High resolution CT chest can provide detailed images of the chest and can be used to evaluate lung involvement, including interstitial lung disease and pulmonary arterial hypertension.
- MRI: MRI can provide detailed images of the internal organs, including the lungs and heart, and can be used to evaluate for organ involvement and disease progression.
- Echocardiography: Echocardiography is a non- invasive imaging test that uses ultrasound waves to produce images of the heart, and is commonly used to evaluate patients with scleroderma for cardiac involvement and pulmonary hypertension.
- Radiocontrast esophagography: This test uses a contrast material and X-rays to evaluate the esophagus and assess for involvement and swallowing difficulties (dysphagia).
- Renal imaging: Renal imaging, such as a renal ultrasound, can be used to evaluate kidney involvement and monitor for scleroderma renal crisis.
In summary, imaging studies play a critical role in the evaluation and management of scleroderma patients, providing information about the extent and progression of disease, and guiding therapeutic decisions.
What is management of Scleroderma?
The management of scleroderma depends on the type and severity of the disease. General management strategies for scleroderma may include:
- Medications: Medications can be used to treat the symptoms of scleroderma, such as pain, stiffness, and fatigue. These may include nonsteroidal anti- inflammatory drugs (NSAIDs), corticosteroids, immunosuppressive drugs, and phosphodiesterase-5 inhibitors.
- Physical therapy: Physical therapy can help improve range of motion, reduce pain. and increase strength n individuals with scleroderma
- Occupational therapy: can help individuals with scleroderma improve their ability to perform daily activities and maintain independence.
- Supportive care: Supportive care measures, such as skin care, wound care, and diet modifications, can help manage the symptoms of scleroderma and prevent complications.
- Monitoring for complications: Regular monitoring by a healthcare provider can help detect and treat complications of scleroderma, such as dysphagia, lung involvement, and kidney involvement.
It is important for individuals with scleroderma to be evaluated and treated early, as the disease can progress and cause significant morbidity and mortality if not properly managed. The management plan should be individualized to meet the specific needs of each person with scleroderma.
What are the complications of scleroderma?
Complications of scleroderma are either related to skin manifestations or related to systemic manifestations involving internal organ like GIT, lungs, heart and kidneys.
Skin manifestations:
Skin related complications are hallmark of scleroderma and mostly the patients are diagnosed clinically with distinct features of skin involvement.

Complications involving hands and toes:
Sclerodactyly: a condition where the skin on the fingers becomes tight, thick and shiny. These symptoms can result in limited joint movement and cause discomfort or pain.
Calcinosis: is the accumulation of calcium deposits in the skin and underlying tissues.
Raynaud’s phenomenon: Spasm of blood vessels of fingers and toes causing discolouration of fingers. The fingers become white in response to vascular spasm when exposed to cold, when spasm is relieved the fingers turn blue and then red. It can lead to permanent impairment of blood supply leading to gangrene.
Auto-amputation: refers to development of digital gangrene followed by shedding of fingers and toes as a consequence of reduced blood supply.
Complications involving face:
Scleroderma can cause facial changes, including tight and thickened skin on the face, loss of skin elasticity, and decreased mobility in the facial muscles.
The skin may also appear shiny and discolored. In severe cases, the disease can cause facial asymmetry and distortion of the features, including the eyes, nose, and mouth. The tightened skin of nose and mouth gives it ‘beaked nose’ and ‘fish mouth’ appearance.
The loss of skin elasticity can cause loss of forehead wrinkles, eyelids to droop, and the mouth to turn down at the corners, leading to a permanent frown.
Sometimes, there is dilatation of blood vessels over face called ‘telangieactasia ‘
These symptoms can result in difficulty speaking, eating, and other activities that require facial movements.
What are advanced complications of Scleroderma?
Advanced complications of scleroderma refer to complications related to organ system including lung, heart, kidney and gut related complications which can be life threatening for the patient.
Lung Complications:
Lung complications are most dreadful and life threatening complications of scleroderma.
Lung fibrosis is a common complication of scleroderma and refers to the development of scar tissue in the lungs, which can lead to:
Decreased lung function: The accumulation of scar tissue reduces the ability of the lungs to expand and contract, causing shortness of breath, wheezing and decreased exercise tolerance.
Alveolar damage: The air sacs in the lungs can be damaged, leading to decreased gas exchange and hypoxia (low oxygen levels).
Pulmonary hypertension: High blood pressure in the lungs can occur as a result of lung fibrosis and may lead to right heart failure.
Interstitial lung disease: The presence of scar tissue in the interstitial spaces of the lungs can cause interstitial lung disease, which is characterized by breathing difficulties, cough and crackles on lung examination.
High-resolution computed tomography (HRCT) can be used to visualize lung fibrosis and assess the extent of lung damage in scleroderma patients. HRCT images can reveal the presence of interstitial thickening, architectural distortion, honeycombing and bullae (air-filled spaces). These findings can help guide treatment and monitoring of disease progression.
The treatment of advanced scleroderma with lung involvement typically involves a combination of approaches, including:
Immunosuppressive therapy: Drugs like methotrexate, cyclophosphamide, and mycophenolate mofetil can help suppress the immune system and slow down the progression of lung fibrosis.
Vasodilators: Drugs like bosentan, sildenafil, and iloprost can help improve blood flow to the lungs and reduce pulmonary hypertension.
Oxygen therapy: Supplemental oxygen can help improve oxygenation in patients with low oxygen levels.
Physical therapy and rehabilitation: Exercise and physical therapy can help improve lung function and overall physical endurance.
Antifibrotic agents: Drugs like pirfenidone and nintedanib can target specific pathways involved in the development of lung fibrosis and have shown promising results in clinical trials. Both these are FDA approved oral medications, but are costly and may be associated with side effects.
Nintedanib: It is a tyrosine kinase inhibitor that targets growth pathways of fibroblasts.
Pirfenidone: This is anti inflammatory and antifibrotic drug which reduces proliferation of fibroblast and inhibits collagen synthesis.
Lung transplantation: In severe cases of lung fibrosis, lung transplantation may be considered as a treatment option.
It is important to note that the treatment of advanced scleroderma with lung involvement is complex and often requires a multidisciplinary approach. The specific treatment plan will depend on the severity of lung involvement, overall health, and the presence of other comorbidities.
Renal involvement in scleroderma:
Renal involvement, or scleroderma renal crisis (SRC), is a severe complication of scleroderma that affects the kidneys. It is characterized by the sudden onset of high blood pressure and rapidly declining kidney function. The exact cause of SRC is not known, but it is thought to be related to changes in blood vessels in the kidneys.
Symptoms of SRC can include:
- High blood pressure: Blood pressure can increase suddenly and dramatically.
- Proteinuria: Increased amounts of protein in the urine, a sign of kidney damage.
- Edema: Swelling due to excess fluid accumulation.
- Decreased urine output: A sign of declining kidney function.
Diagnosis of SRC typically involves blood tests, urine tests, and imaging studies. Treatment of SRC typically involves controlling high blood pressure and treating any underlying kidney damage. This may include medications such as ACE inhibitors, ARBS, and diuretics, as well as other measures to support kidney function. In severe cases, dialysis or kidney transplantation may be necessary.
It is important for patients with scleroderma to be regularly evaluated for kidney involvement by a specialist, as early detection and treatment of SRC can greatly improve outcomes.
Dysphagia in Scleroderma:
Dysphagia, or difficulty swallowing, is a common complication of scleroderma. It can be caused by a number of factors, including:
- Esophageal involvement: Scleroderma can cause the esophagus to become stiff and narrow, making it difficult for food and liquids to pass through.
- Muscle weakness: Scleroderma can cause muscle weakness in the face, neck, and upper chest, making it difficult to move food and liquids into the esophagus.
- Dysphagia can lead to malnutrition, dehydration, and aspiration (inhalation of food or liquid into the lungs), which can lead to pneumonia. Treatment of dysphagia in scleroderma may involve medications to help relax the esophagus and improve swallowing, as well as changes to the consistency and temperature of foods. In severe cases, dilation (stretching) of the esophagus or surgical intervention may be necessary.
- Gastric involvement:
It is important for patients with scleroderma to be properly evaluated for dysphagia and digestive system involvement.
What is prognosis and life expectancy in Scleroderma?
The life expectancy of individuals with scleroderma can vary greatly depending on the type and severity of the disease, as well as other factors such as age, overall health, and the presence of comorbidities.
In general, patients with limited cutaneous scleroderma (affecting only the skin) have a better prognosis and a normal life expectancy. In contrast, those with diffuse cutaneous scleroderma (involving skin and internal organs) and systemic sclerosis (involving multiple organs) can have a more serious course with a shorter life expectancy.
In patients with systemic sclerosis, the presence of lung involvement, especially interstitial lung disease, is associated with a poorer prognosis and a reduced life expectancy. Other factors that can affect life expectancy include the presence of Raynaud’s phenomenon, high blood pressure in the lungs (pulmonary hypertension), and kidney involvement.
It is important to note that advances in medical treatment and management of scleroderma have improved outcomes and life expectancy for many patients in recent years. Regular monitoring and treatment by a specialist can help manage symptoms and improve overall prognosis.
Who can help a patient with Scleroderma?
- A physician
- A rheumatologist
- Physical therapist
- Multidisciplinary team in case of diffuse systemic involvement
